Patient Safety: The Foundation of Care
January 29, 2026
From pediatrics to geriatric care, all patients are affected by the choices their healthcare practitioners make. Clinical decisions, medications dispensed, and every treatment delivered carry the potential to help or harm.
At Chapman University School of Pharmacy, faculty have spent more than a decade advancing patient safety through research that addresses real-world risks, from medication errors during hospital transitions to bias in artificial intelligence prescribing tools.
“Patient safety is not theoretical,” Laressa Bethishou, Pharm.D., said. “It’s practiced, measured, and continuously improved at every level of care.”
What Is Patient Safety?
 Patient safety refers to the prevention of errors and adverse effects associated with healthcare. It encompasses the coordinated efforts of professionals, institutions, and systems to reduce the risk of harm throughout a patient’s care journey, from preventing medication errors to improving continuity across care settings and minimizing unintended harm from new therapies or technologies.
Patient safety refers to the prevention of errors and adverse effects associated with healthcare. It encompasses the coordinated efforts of professionals, institutions, and systems to reduce the risk of harm throughout a patient’s care journey, from preventing medication errors to improving continuity across care settings and minimizing unintended harm from new therapies or technologies.
At its core, patient safety means delivering the right care, at the right time, in the right way, every single time.
Chapman faculty address patient safety across this spectrum, from frontline clinical practice to international policy development.
Why Patient Safety Matters
According to the World Health Organization, medical errors remain a leading cause of injury and death in healthcare settings. Failures in patient safety may lead to prolonged illness and preventable readmissions, medication-related harm, permanent disability or loss of life, emotional and financial burdens on families, moral distress among healthcare professionals, and erosion of trust in healthcare systems.
Effective patient safety practices improve outcomes, reduce costs, and strengthen confidence in care delivery.
Chapman’s Approach to Patient Safety
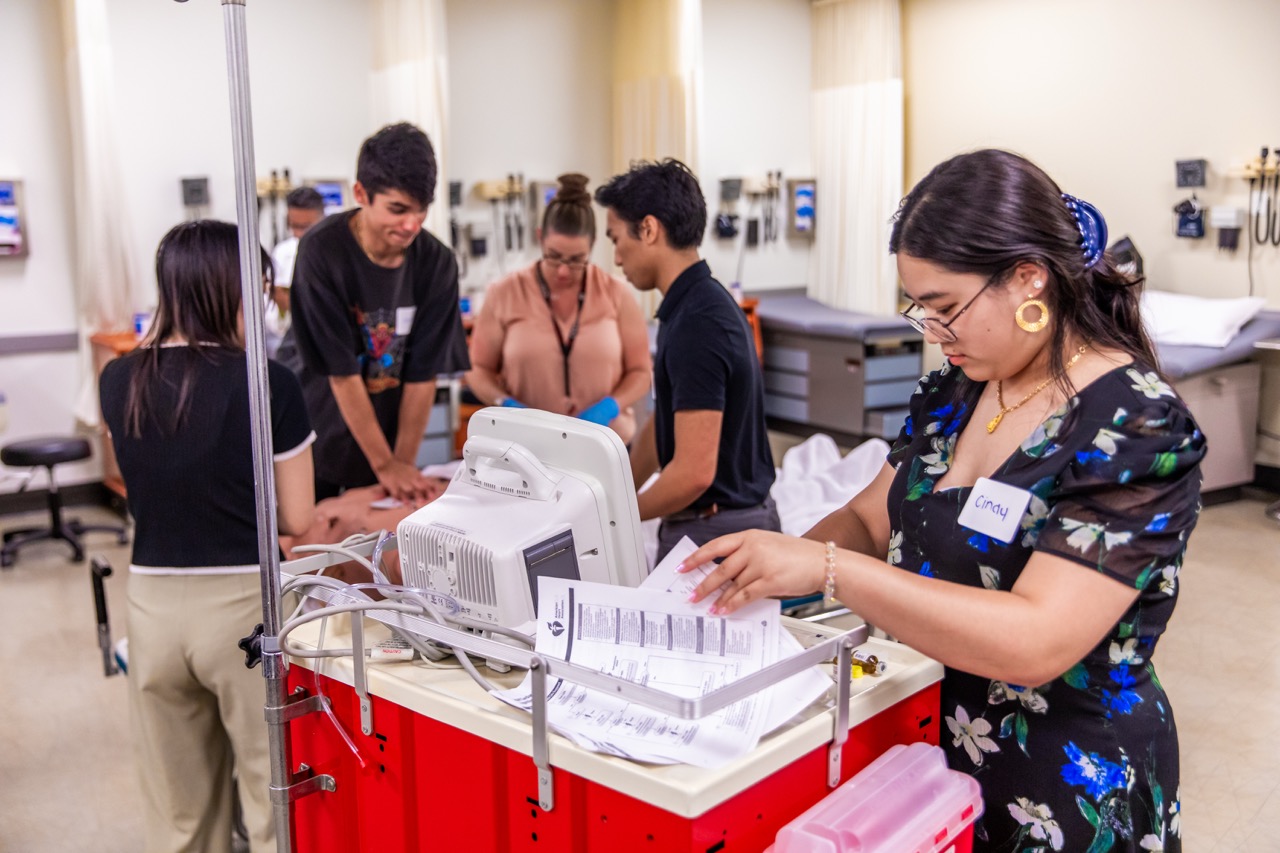 CUSP approaches patient safety as a shared responsibility that spans research, education, clinical practice, and policy.
CUSP approaches patient safety as a shared responsibility that spans research, education, clinical practice, and policy.
Faculty research addresses systemic vulnerabilities that place patients at risk. Sherry Wang, Ph.D., examines how artificial intelligence tools used in opioid prescribing can unintentionally perpetuate bias or misclassify patients when algorithms lack transparency. Her widely cited research on opioid risk scoring systems, including NarxCare®, has demonstrated how opaque AI models can introduce safety risks by influencing prescribing decisions without clear accountability.
“We need to understand not just what these algorithms do, but how they make decisions,” Wang said. “Without transparency, we can’t ensure they’re making patients safer.”
Through her NIH-funded AIM-AHEAD project, Wang leads national efforts to assess and reduce bias in machine learning models used in opioid prescribing, ensuring that technology improves safety and access rather than restricting care.
The Pharmacist’s Role in Patient Safety
Pharmacists serve as essential guardians of patient safety, and are often the final checkpoint before medications reach patients to play a critical role in identifying risks.
The contributions to patient safety by Jerika Lam, Pharm.D., highlights the pharmacist’s responsibility in promoting patient safety at the global level. As a co-author of the International Pharmaceutical Federation’s Statement of Policy on the Role of Pharmacists in Promoting Patient Safety and a member of its Patient Safety Policy Committee, Lam has helped define international standards for how pharmacists safeguard patients across healthcare systems.
At Chapman University, her leadership as faculty advisor to Chapman’s California Society of Health-System Pharmacists/American Society of Health-System Pharmacists student chapter has translated safety principles into action. Student-led initiatives under her mentorship, including nationally recognized COVID-19 response efforts and naloxone education programs, directly addressed community risk, medication safety, and harm reduction.
Building a Culture of Safety
Beyond individual vigilance, patient safety mandates a culture where professionals feel empowered to speak up, question assumptions, and learn from error.

“Patients are particularly vulnerable when moving between hospitals, skilled nursing facilities, and outpatient care,” says Bethishou. “Medication discrepancies and communication failures commonly occur during these transitions.”
Through direct patient care, pharmacist-led practice models, and highly cited research on continuity of care, Bethishou has demonstrated how structured pharmacist interventions reduce medication errors and prevent avoidable readmissions. Her service on the American Society of Consultant Pharmacists’ Transitions of Care Medication Safety Committee and leadership roles within the Patient Safety Movement Foundation ensure that evidence-based practices are translated into national guidance and educational resources.
In addition, Bethishou co-chairs the Pacific Coast Patient Safety Conference, an annual meeting to promote safety, equity, and collaboration across all levels of care. Created by Chapman University in 2019, California Society of Health-System Pharmacists has since joined as co-host to encourage greater engagement in CE programming, peer-reviewed case studies, and interactive policy discussions, all centered around integrating evidence-based safety measures into practice.
The Patient Voice in Healthcare
A defining feature of Chapman’s patient safety philosophy is the belief that patients must be active and empowered partners in their care.
Faculty research and practice emphasize listening to patients, addressing real-world barriers, and ensuring continuity across care settings. Bethishou’s work highlights how gaps in communication during care transitions can undermine safety and patient trust, while pharmacist involvement restores continuity and empowers patients to understand and manage their medications safely.
“Students learn to view patients not as passive recipients of care, but as essential collaborators whose insights are critical to safety,” Lam said.
Innovation in Drug Safety and Precision Medicine
Patient safety also depends on safer therapies. Keykavous Parang, Pharm.D., Ph.D., researches advance medication safety through precision drug design.
 His research on peptide–drug conjugates in oncology addresses the systemic toxicities associated with traditional chemotherapy, particularly cardiotoxicity linked to drugs such as doxorubicin. By improving tumor targeting, controlling drug release, and reducing off-target exposure, this research enhances therapeutic efficacy predictability while minimizing harm to healthy tissue.
His research on peptide–drug conjugates in oncology addresses the systemic toxicities associated with traditional chemotherapy, particularly cardiotoxicity linked to drugs such as doxorubicin. By improving tumor targeting, controlling drug release, and reducing off-target exposure, this research enhances therapeutic efficacy predictability while minimizing harm to healthy tissue.
These innovations reflect Chapman’s commitment to improving patient safety not only through systems and policy, but through the development of safer medicines themselves.
The Future of Patient Safety Starts at Chapman
As healthcare grows more complex, patient safety challenges continue to evolve. From ethical AI and opioid safety to continuity of care and precision therapeutics, Chapman faculty are shaping the future of patient safety at every level of healthcare.
CUSP prepares students not only to deliver care, but to protect patients, challenge unsafe systems, and lead change. Through the Doctor of Pharmacy program, our 3 graduate degree programs, and by providing professional development and continuing education opportunities, Chapman equips healthcare professionals with the skills, judgment, and ethical grounding necessary to make healthcare safer for everyone.
“Patient safety isn’t just a concept we teach. It’s something we actively research, practice, study, and advance every day,” Parang said. “Because every patient deserves care that heals without harm.”


